Uterine Fibroid Embolization (UFE)
Do you have painful fibroids but aren’t ready for a hysterectomy? You’ve got options.
Uterine fibroids are most common in women in their 30s.
What are uterine fibroids?
Uterine fibroids are firm, muscular growths in the uterus that can range from undetectable by the human eye to the size of a melon. They can be single or in clusters. Some never cause symptoms and remain undetected, while others disrupt the woman’s life. You may never know you have a fibroid until you have symptoms, but if you have symptoms, you dread the monthly pain and heavy bleeding.
As many as 50% of women in their reproductive years have fibroids.
Fibroids are more than a “bad” period
It’s hard to explain to anyone who hasn’t experienced it. Fibroids do more than make your period “worse.” They cause a range of symptoms that can depend on the location, number, and size of the fibroids. For some women, a heavy period is just the beginning. Excessive bleeding, extra-long periods, pelvic pain, frequent urination, constipation, back and leg pain – fibroids can be debilitating.
As many as 80% of women develop fibroids by age 50.
What is Uterine Fibroid Embolization (UFE)?
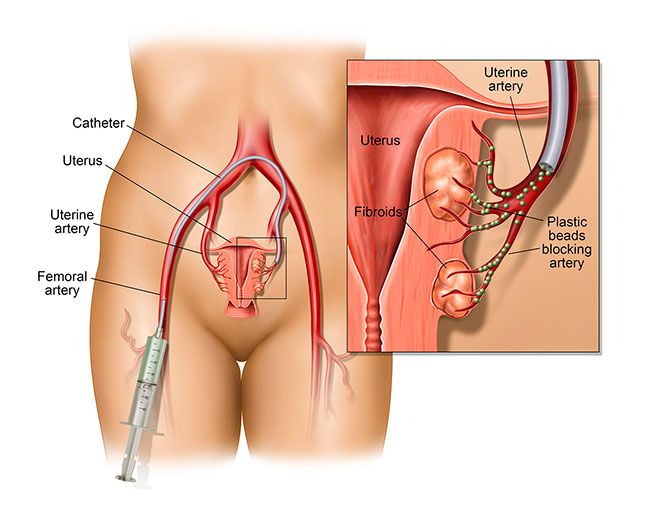
UFE addresses the fibroid problem without removing the uterus. UFE is a minimally invasive procedure done as an outpatient procedure under mild IV sedation. The physician uses X-ray guidance to thread a catheter through a small incision in the groin and guide it into the uterus. Then, an injection of microspheres cuts off the blood flow to the fibroids, essentially starving them. With their supply cut off, they shrink, relieving your symptoms.
Interventional radiologists have performed UFE to treat uterine bleeding since the 1970s. It’s a safe, effective, proven method of treating symptomatic fibroids.
UFE relieves fibroid symptoms without the complications, side effects, recovery time, and decreased sexual function associated with hysterectomy.
UFE completely or significantly relieves fibroid-related symptoms in almost 90% of women who try it.
How soon will you feel relief?
Symptom relief is noticeable within a few days. The fibroids continue to shrink for several months, and by six months post-UFE, your symptoms will have stabilized.
Women who undergo UFE can typically go home the same day and can expect to resume normal activities in one to two weeks.
Many women who had a hysterectomy for fibroids didn’t know they had another option.
You’ve got options! If you’ve been told you need a hysterectomy for your fibroids, call for a second opinion. Many hysterectomies simply aren’t necessary when UFE is an option.
If you’re living with the debilitating symptoms of fibroids, call us at +1 262-656-2508 for a consultation. We’d be happy to discuss your options and whether UFE is right for you.